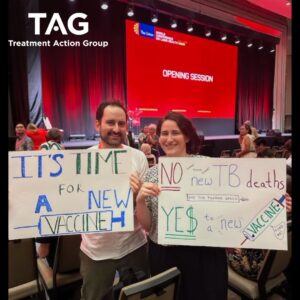
It’s Time to Stop the World’s Oldest Pandemic: We Need a New TB Vaccine
12 November 2024
This week, experts and policymakers are convening at the Union’s World Conference on Lung Health to discuss tuberculosis (TB), the world’s deadliest and most neglected infectious disease. Since the turn of the 20th century, over one billion people have died from TB – a death toll greater than that from malaria, smallpox, HIV/AIDS, cholera, plague and influenza combined.
The official UN target to reduce TB deaths by 75% between 2015 and 2025 is now out of reach. Many commentators believe that the 2030 target of reducing TB by 90% will prove elusive too – unless we see an urgent increase in investments in new tools that will make a dent in the curve of the epidemic.
Promising TB vaccine pipeline
TB scientific advances over the past five years are dramatically improving the way the disease is treated and, just as importantly, they are moving the needle on a long-awaited vaccine, which history suggests will be needed to effectively end TB as a public health crisis.
The 100 year-old BCG (Bacillus Calmette-Guérin) vaccine is still the world´s only vaccine against TB. It is mainly given to babies and young children to prevent more serious forms of TB, such as TB meningitis which affects the brain. However, the vaccine is essentially ineffective for the more than nine million adults and adolescents who develop TB each year.
This could all change in the coming years if one of the three preventative vaccines now in Phase III trials – the IAVI and Biofabri-sponsored MTBVAC, the Gates Medical Research Institute supported M72/AS01E vaccine, and the Serum Institute’s VPM1002 candidate – demonstrates safety and efficacy.
However adequate funding will be needed to make this a reality. Unfortunately, adequate funding is not something TB – a disease that disproportionately affects the world’s poorest populations – has ever had.
The science has brought us this far and now it’s time to finish the job – we can’t afford to wait another hundred years to finally deliver a broadly effective vaccine. As we await results from clinical trials, we also need to begin preparing now for the rollout of successful vaccine candidates.
Avoiding TB vaccine inequity
A clear understanding of the scale of demand for TB vaccines will be essential to ensure adequate manufacturing capacity is built and sustained to deliver required doses once a new TB vaccine is licensed by regulators and recommended by public health authorities. This is new terrain for the TB response and will be a costly endeavour, requiring significant lead time.
The COVID-19 response provided some valuable insights as to what could be accomplished with adequate investment in clinical development, de-risking of manufacturing scale up, and broad delivery of vaccines. At the same time, it shined a spotlight on inequities in supply across vaccine-producing and non-producing countries and spurred a movement for sovereign regional manufacturing.
TB Vaccine Accelerator Council
The TB Vaccine Accelerator Council – announced last year by the World Health Organization (WHO) in partnership with Ministers of Health from several high-burden countries, investment banks, and leading philanthropic organizations – could help lay the groundwork in the years to come for the effective rollout of new TB vaccines, principally to people living in countries where the prevalence of the disease is highest. It must deliver this goal with the urgency of the COVID response, but with an unwavering commitment to equity that the COVID response lacked.
The efforts of the Council were boosted earlier this year when Gavi, the Vaccine Alliance, decided to include TB vaccines as part of its Vaccine Investment Strategy. Gavi financing will provide a critical lifeline to ensure TB vaccine availability in the 54 Gavi-eligible countries.
Gavi support will be instrumental, not only in securing the resources these countries need to finance vaccine procurement, but will also support the establishment of delivery pathways to reach adult and adolescent populations who are critical in stemming the tide of new TB infections but fall outside of routine childhood immunization programs.
Challenges facing high-burden countries
In parallel, however, strategies are needed to support access to TB vaccines in those middle-income countries (MICs) that have transitioned, are transitioning, or were never eligible for Gavi support but face the greatest burden of TB disease.
These strategies must include investment in vaccine delivery platforms and mechanisms for countries to pool purchasing, including regionally, to leverage their collective volumes for better negotiating power. All of us convening at the Union Conference this week should also think about policy solutions that would indirectly allow MICs in invest more in health systems and vaccine delivery, including sovereign debt forgiveness and relief.
According to WHO, accelerating the scale up of vaccines would prevent up to 76.6 million cases, while producing between $372 billion in economic benefits by 2050. But more importantly, as TB survivor and advocate Kate O’Brien has reminded us—the most important resources are human lives. Each year we stall, each year we fail to muster the investment and political will that TB deserves, more than a million lives are lost. Working together, we can and must stop this from happening.
By Shelly Malhotra and Mike Frick

Shelly Malhotra is Vice President for External Affairs and Global Access at IAVI. She has over two decades of experience in global health focused on harnessing public-private partnerships to facilitate access to innovations.

Mike Frick is a Co-Director of the Tuberculosis program at the Treatment Action Group (TAG). He has been advancing access to preventive options for tuberculosis for over a decade.
Source: Health Policy Watch