How DNA Tricks Help TB Fight Back Against Treatment
5 December 2025
Researchers are opening up new possibilities for tracking and treating tuberculosis by revealing hidden DNA changes that allow the deadly bacterium to adapt, spread and resist drugs.
Tuberculosis (TB) is one of the oldest and deadliest infectious diseases we know. It commonly impacts the lungs, but can also affect other areas of the body like the spine, brain or kidneys.
In fact, Egyptian mummies have been found with skeletal deformities typical in untreated TB infection, which even feature in Egyptian art.
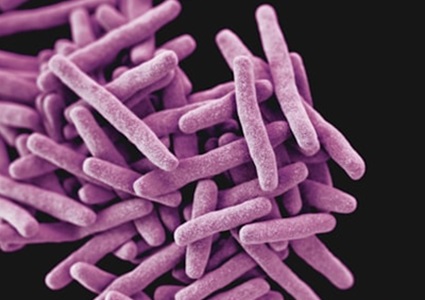
Caused by the bacterium Mycobacterium tuberculosis, in the 21st Century, TB still kills more than a million people every year. Yet our understanding of how it continues to be so deadly has remained out of reach.
Antibiotics were first developed to treat TB in the 1940s, but the bacteria soon began to develop drug resistance. Some strains have also developed multidrug resistance, making them even more difficult to treat.
For decades, we’ve studied the bacterium’s DNA to understand how it evolves drug resistance, but the tools we relied on couldn’t find an important part of the story.
In our latest study, published in Nature Communications, we’ve used new techniques to identify previously unknown genetic variations of M. tuberculosis, to create a more complete map of the genome and unlock potential treatment targets.
Tuberculosis surveillance
Traditional short-read DNA sequencing is the backbone of global pathogen surveillance. It identifies small genetic mutations that drive the evolution of drug resistance and helps track outbreaks.
But short reads of DNA sequence struggle to accurately represent the most complex regions of the TB genome – areas full of repetitive sequences, mobile elements and large rearrangements.
Until recently, most of these large structural DNA changes, also known as structural variants, were effectively invisible.
Our new study used cutting-edge long-read DNA sequencing together with genome graph analysis to find genetic variations that were previously inadvertently missed.
In place of the traditional single reference genome, these new techniques allowed us to represent and compare the full genetic diversity within strains of the M. tuberculosis species for the first time.
This collection of genetic sequences forms the first n M. tuberculosis pangenome, a way of representing all the genetic variation in a species, rather than describing just one example of it.
This is important because one strain of M. tuberculosis might cause only mild disease in a person, while another strain with antibiotic-resistance mutations or differences in virulence could lead to more severe disease or be harder to treat.
Using this more flexible, expansive framework allowed us to map and compare parts of the bacterial genome that short-read methods consistently miss.
Then, we started seeing things we’d never been able to see before.
DNA rearrangements and antibiotic resistance
The long-read data revealed large structural changes across the genome – deletions, duplications, insertions and inversions that can reshape the bacterium’s biology.
Many of these rearrangements are driven by a small piece of DNA called IS6110, which can move around the genome and trigger dramatic changes in the surrounding DNA.
By mapping these genetic variations, we could trace their origins, how often they occur and the effects they have on different M. tuberculosis strains.
What matters most is how these structural variants influence the bacterium’s ability to adapt, spread and resist antibiotics.
Using computational analysis, we found that particular rearrangements are associated with distinct drug resistance profiles.
Some structural variants affect how many copies of a gene are present. For example, by completely deleting a gene, some strains would be unable to metabolise a drug and so totally escape being killed by it.
Others disrupt regulatory elements – the parts of the genome that control when, where and how much a gene is active.
These kinds of genomic shifts offer M. tuberculosis an alternative way to survive drug treatment, one that cannot be detected by looking only at small DNA mutations.
This helps explain why some TB isolates behave differently than expected when based only on their known small mutations.
It also suggests that structural variation plays a more active role in shaping the long-term evolution of drug resistance than we previously knew.
One of the most striking aspects of our findings is how much important biology was hiding in DNA regions we’d previously ignored.
When research focuses only on single-nucleotide changes (the kinds that affect just one spot on the DNA) the rest of the genome can look silent.
But once long-read sequencing opened up those difficult regions, we found they have been alive with evolutionary activity all along.
Understanding ‘invisible’ DNA changes
TB remains a persistent threat, and drug-resistant strains are among the most difficult and expensive infections to treat.
By revealing structural variants linked to resistance, our work offers new clues for improving prediction models and refining diagnostic tools.
If we can identify these larger genomic changes in clinical samples, we may be able to better anticipate which strains are likely to fail treatment or spread drug-resistant forms of the disease.
This is important for providing patients with the right combination of drugs to help treat their specific infection.
This research also has major implications for surveillance.
Public health programs worldwide rely on genomic data to monitor TB transmission and resistance trends.
Integrating long-read sequencing and pangenomic methods into these programs could provide a far clearer and more accurate view of how the bacterium is evolving in real time.
As long-read technology becomes cheaper and more scalable, this is increasingly feasible.
While our study is computational and laboratory-based, its consequences will ultimately reach the clinic.
More accurate genomic interpretation can strengthen treatment decisions, guide the development of new diagnostics and help health systems stay ahead of emerging resistant strains.
In a disease where delayed diagnosis can have major impacts, better genomic resolution can translate directly into better outcomes.
Better tools for treating and tracking disease
This project represents a shift in how we study TB.
Instead of treating the genome as a fixed reference, we’re beginning to treat it as a landscape – one that changes, rearranges and adapts under selective pressure.
Long-read sequencing and pangenomics let us see this landscape in full.
There is still much to uncover.
The next steps for the field involve integrating these structural variants into resistance prediction models, expanding the pangenome graph with even more diverse isolates and working with collaborators to explore how these genomic changes influence transmission and survival.
The goal is to make structural variant analysis a routine part of TB genomics, rather than a specialised research tool.
These findings have uncovered genetic changes in tuberculosis that were previously invisible, opening the door to better tools for detecting and treating drug-resistant forms of this disease – and hopefully others.
This visibility is crucial because we can only fight what we can see.
By Aleix Canalda Baltrons, Doherty Institute, University of Melbourne
Source: University of Melbourne
SEE ALSO:
- Bioengineer.org: Genome Graphs Uncover Key TB Evolution Insights